Infertility can be a challenging issue for many couples. Male fertility is a significant factor in this challenge. Determining male fertility involves a series of tests and examinations performed by healthcare professionals. This article aims to provide a comprehensive overview of the tests used to assess male fertility.
Introduction to Male Fertility
Male fertility refers to a man’s ability to cause pregnancy in a fertile female. It depends on the quality and quantity of sperm. When a couple struggles to conceive, both partners should undergo medical evaluations to identify potential issues. Male fertility tests are crucial in diagnosing and treating infertility problems.
Initial Consultation and Medical History
Medical History
The first step in assessing male fertility is a thorough medical history. The doctor will ask about past illnesses, surgeries, medications, and lifestyle factors. Understanding the patient’s medical background helps identify potential causes of infertility.
Physical Examination
A physical examination is performed to check for any abnormalities in the reproductive organs. The doctor will examine the penis, scrotum, and testicles. They will look for signs of infections, structural problems, or other issues that might affect fertility.
Semen Analysis
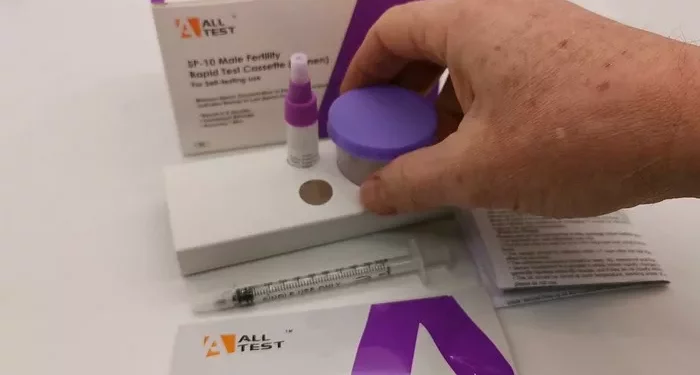
Collection of Semen Sample
A semen analysis is one of the most critical tests in assessing male fertility. The patient provides a semen sample, usually collected through masturbation. It is essential to follow the doctor’s instructions carefully to ensure an accurate sample.
Analyzing the Semen Sample
The semen sample is analyzed in a laboratory to assess various parameters. These include:
Sperm Count: The number of sperm in the semen. A low sperm count can reduce the chances of fertilization.
Sperm Motility: The ability of sperm to move. Poor motility can hinder the sperm from reaching the egg.
Sperm Morphology: The shape and structure of the sperm. Abnormal sperm can have difficulty penetrating and fertilizing the egg.
Semen Volume: The amount of semen produced. Low semen volume can indicate problems with the seminal vesicles or prostate gland.
pH Level: The acidity or alkalinity of the semen. Abnormal pH levels can affect sperm function.
White Blood Cells: The presence of white blood cells can indicate an infection or inflammation.
Hormonal Evaluation
Key Hormones Involved
Hormones play a crucial role in regulating male fertility. The doctor may order blood tests to measure hormone levels, including:
Testosterone: The primary male sex hormone responsible for sperm production.
Follicle-Stimulating Hormone (FSH): Stimulates sperm production in the testes.
Luteinizing Hormone (LH): Stimulates testosterone production.
Prolactin: Elevated levels can interfere with testosterone production and sperm development.
Estradiol: An imbalance in this estrogen hormone can affect sperm production.
Interpreting Hormonal Results
Abnormal hormone levels can indicate various issues, such as hypogonadism, pituitary disorders, or other endocrine problems. The doctor will interpret the results and recommend appropriate treatments or further testing.
See Also: What You Need to Know About Fertility Testing
Genetic Testing
Types of Genetic Tests
Genetic abnormalities can also cause male infertility. The doctor may recommend genetic testing to identify specific conditions, such as:
Karyotyping: Analyzing chromosomes to detect genetic disorders like Klinefelter syndrome.
Y Chromosome Microdeletion Testing: Identifying missing segments of the Y chromosome that affect sperm production.
Cystic Fibrosis Gene Mutation Testing: Certain mutations can lead to congenital bilateral absence of the vas deferens (CBAVD), affecting sperm transport.
Implications of Genetic Findings
Genetic tests can provide valuable insights into the underlying causes of infertility. Understanding these causes can guide treatment options and inform decisions about assisted reproductive technologies.
Imaging Studies
Scrotal Ultrasound
A scrotal ultrasound is a non-invasive imaging test used to examine the testicles and surrounding structures. It helps detect:
Varicocele: Enlarged veins in the scrotum that can impair sperm production.
Hydrocele: Fluid accumulation around the testicle.
Tumors: Abnormal growths that may affect fertility.
Obstructions: Blockages in the reproductive tract.
Transrectal Ultrasound (TRUS)
TRUS is used to examine the prostate gland and seminal vesicles. It helps identify obstructions or abnormalities that may interfere with semen production or ejaculation.
Magnetic Resonance Imaging (MRI)
In some cases, an MRI may be needed to provide detailed images of the reproductive organs and surrounding structures. It is useful for detecting complex abnormalities that other imaging tests might miss.
Testicular Biopsy
Procedure
A testicular biopsy involves taking a small tissue sample from the testicle. This procedure is usually performed under local anesthesia. There are two main types:
Percutaneous Biopsy: Using a needle to extract a tissue sample.
Open Biopsy: Making a small incision in the scrotum to access the testicle and obtain a tissue sample.
Analyzing the Biopsy Sample
The tissue sample is examined under a microscope to assess sperm production and identify any abnormalities in the testicular tissue. A biopsy can help diagnose conditions like:
Spermatogenic Failure: The inability of the testicles to produce sperm.
Obstructions: Blockages preventing sperm from reaching the semen.
Testicular Cancer: Malignant growths affecting sperm production.
Specialized Tests
Anti-Sperm Antibody Testing
In some cases, the immune system may produce antibodies that attack sperm, impairing their function. Anti-sperm antibody testing detects these antibodies in the blood, semen, or cervical mucus. High levels of anti-sperm antibodies can cause infertility by:
Impairing Sperm Motility: Preventing sperm from swimming effectively.
Blocking Sperm Penetration: Hindering sperm from entering and fertilizing the egg.
Sperm DNA Fragmentation Test
This test measures the integrity of sperm DNA. High levels of DNA fragmentation can affect fertilization and embryo development. Causes of sperm DNA fragmentation include:
Oxidative Stress: Damage from reactive oxygen species (ROS).
Infections: Inflammatory responses affecting sperm DNA.
Lifestyle Factors: Smoking, poor diet, and exposure to toxins.
Oxidative Stress Test
Oxidative stress can damage sperm and impair fertility. This test measures the levels of reactive oxygen species (ROS) in the semen. High ROS levels can indicate:
Infections: Causing inflammation and oxidative stress.
Varicocele: Leading to increased ROS production.
Environmental Factors: Exposure to pollutants and toxins.
Advanced Imaging Techniques
Computer-Assisted Semen Analysis (CASA)
CASA uses computer algorithms to analyze semen samples with high precision. It provides detailed information on sperm motility, morphology, and concentration. CASA helps:
Standardize Semen Analysis: Reducing human error and variability.
Enhance Diagnostic Accuracy: Providing more reliable results.
Electron Microscopy
Electron microscopy offers highly detailed images of sperm and testicular tissue. It helps identify:
Ultrastructural Abnormalities: Detailed structural defects in sperm.
Sperm Function Issues: Problems at the microscopic level affecting fertility.
Lifestyle and Environmental Factors
Impact of Lifestyle Choices
Lifestyle choices can significantly affect male fertility. The doctor may discuss factors like:
Diet and Nutrition: A balanced diet supports healthy sperm production.
Exercise: Regular physical activity can improve fertility.
Alcohol and Drug Use: Excessive consumption can impair sperm quality.
Smoking: Reduces sperm count and motility.
Stress Management: Chronic stress can affect hormone levels and fertility.
Environmental Exposures
Exposure to environmental toxins and pollutants can impact fertility. The doctor may inquire about:
Occupational Hazards: Jobs involving exposure to chemicals or radiation.
Heat Exposure: Frequent exposure to high temperatures can affect sperm production.
Chemical Exposure: Pesticides, heavy metals, and other toxins can impair fertility.
Conclusion
Assessing male fertility involves a comprehensive approach, including medical history, physical examination, semen analysis, hormonal evaluation, genetic testing, imaging studies, and specialized tests. Understanding the various factors that affect male fertility is crucial for accurate diagnosis and effective treatment. If you are facing challenges with fertility, consulting a healthcare professional can provide the necessary guidance and support.
By addressing underlying issues and making informed lifestyle choices, many men can improve their fertility and achieve their goal of starting a family.
Related Links: