Testicular cancer is a rare but significant concern for men, particularly those in their prime reproductive years. Despite its rarity, the impact of testicular cancer on fertility is a critical issue. Understanding whether testicular cancer causes sterility involves looking at the disease itself, the treatments available, and the physiological impacts on the male reproductive system.
See Also: Can Low White Blood Cells Cause Infertility?
Testicular Cancer Overview
What is Testicular Cancer?
Testicular cancer occurs in the testes, which are part of the male reproductive system. The testes produce sperm and the hormone testosterone. Testicular cancer is most commonly diagnosed in men between the ages of 15 and 35, though it can occur at any age. There are two main types of testicular cancer: seminomas and non-seminomas, each with different characteristics and treatment responses.
Causes and Risk Factors
The exact cause of testicular cancer remains unknown, but several risk factors have been identified. These include:
- Cryptorchidism: Undescended testicles increase the risk.
- Family History: A family history of testicular cancer can heighten risk.
- Age: It primarily affects younger men.
- Race and Ethnicity: More common in white men compared to men of other races.
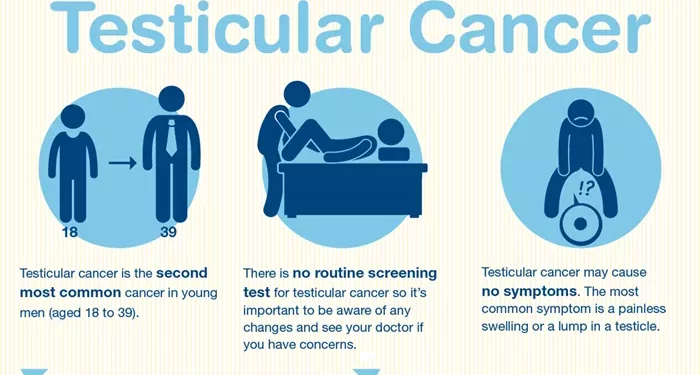
Symptoms
Early detection is crucial. Symptoms can include:
- A lump or swelling in the testicle.
- Pain or discomfort in the scrotum or testicle.
- A feeling of heaviness in the scrotum.
- A dull ache in the lower abdomen or groin.
- Sudden fluid collection in the scrotum.
Testicular Cancer and Fertility
Direct Effects on Fertility
Testicular cancer itself can affect fertility in several ways. The tumor can damage the tissue of the testicle, potentially impairing sperm production. This is particularly significant if both testicles are affected, though this is rare. In cases where only one testicle is affected, the remaining healthy testicle often compensates by producing sufficient sperm and testosterone.
Impact of Treatment
The primary treatments for testicular cancer include surgery, radiation therapy, and chemotherapy. Each of these treatments has potential effects on fertility.
Surgery
Orchiectomy
The standard surgical treatment for testicular cancer is an orchiectomy, which involves the removal of the affected testicle. Men with one healthy testicle generally retain normal fertility and testosterone levels. However, the loss of one testicle may lead to a decrease in sperm production, though not necessarily to the point of sterility.
Retroperitoneal Lymph Node Dissection (RPLND)
RPLND is a more complex surgery that removes lymph nodes in the abdomen. This surgery can sometimes damage nerves involved in ejaculation, potentially causing retrograde ejaculation. This condition, where semen enters the bladder instead of exiting through the urethra, can lead to infertility.
Radiation Therapy
Radiation therapy targets and kills cancer cells. When used for testicular cancer, it is typically directed at the abdominal lymph nodes. Although less commonly used now for testicular cancer, radiation can damage sperm cells and lower sperm count. The remaining testicle may be shielded during treatment, but some collateral damage can occur, affecting fertility.
Chemotherapy
Chemotherapy uses drugs to kill cancer cells throughout the body. It is particularly effective against testicular cancer but can also impact fertility. Chemotherapy drugs can reduce sperm production and cause DNA damage in sperm cells. The extent of the impact depends on the type and dosage of chemotherapy drugs used. While sperm production often recovers after treatment, in some cases, it may not return to pre-treatment levels.
Long-Term Fertility Concerns
Sperm Production and Quality
After treatment for testicular cancer, many men experience a temporary reduction in sperm count and motility. Recovery times vary; some men may see a return to normal levels within a year, while others may take longer. In certain cases, especially after high doses of chemotherapy or extensive radiation therapy, sperm production may not fully recover, leading to long-term fertility issues.
Hormonal Changes
Testicular cancer and its treatments can also affect hormonal balance. The testes produce testosterone, which is essential for sperm production. Loss of one testicle usually does not significantly impact testosterone levels. However, if both testicles are affected or removed, testosterone replacement therapy may be necessary, which can also influence fertility.
Psychological Impact
The psychological effects of a cancer diagnosis and its treatment can also impact fertility. Stress, anxiety, and depression can affect libido and sexual function, indirectly influencing fertility. Psychological support and counseling can be beneficial in managing these aspects.
Fertility Preservation Strategies
Sperm Banking
Before starting treatment, men are often encouraged to bank sperm. Sperm banking involves collecting and freezing sperm samples for future use. This is a reliable method to preserve fertility and provides an option for men to father biological children through assisted reproductive techniques later.
Testicular Sperm Extraction (TESE)
For men who do not have viable sperm in their ejaculate after treatment, TESE is an option. This procedure involves extracting sperm directly from the testicular tissue. It can be used in conjunction with in vitro fertilization (IVF) to achieve pregnancy.
Hormonal Treatments and Supplements
In some cases, hormonal treatments and supplements can help restore sperm production. These treatments aim to stimulate the testes to produce sperm or improve the overall hormonal balance.
Assisted Reproductive Techniques
In Vitro Fertilization (IVF)
IVF involves combining eggs and sperm outside the body to create embryos, which are then implanted in the uterus. This technique can be used with sperm from sperm banking or TESE. IVF has a high success rate and is a common option for men who have undergone treatment for testicular cancer.
Intracytoplasmic Sperm Injection (ICSI)
ICSI is a specialized form of IVF where a single sperm is injected directly into an egg. This technique is particularly useful when sperm count or motility is very low. It maximizes the chances of fertilization even with a limited number of sperm.
Case Studies and Research Findings
Case Study 1: Post-Chemotherapy Fertility
A study followed 500 men treated for testicular cancer with chemotherapy. It found that approximately 80% of the men regained normal sperm production within five years. However, 20% experienced persistent low sperm counts or azoospermia (no sperm). The study highlights the importance of sperm banking before treatment.
Case Study 2: Impact of Radiation Therapy
Research involving men who underwent radiation therapy for seminoma showed mixed results regarding fertility. While many regained normal sperm counts within two years, some experienced long-term reductions. The use of shielding techniques during radiation was found to be crucial in preserving fertility.
Case Study 3: Fertility Outcomes After Orchiectomy
A study on men who had undergone orchiectomy alone (without additional treatments) found that most retained normal fertility. The remaining testicle typically compensated for the loss. However, those with pre-existing low sperm counts or other fertility issues before the diagnosis were more likely to experience fertility challenges post-surgery.
Prevention and Early Detection
Self-Examination
Regular self-examination can help detect testicular cancer early. Men should be encouraged to perform monthly self-exams to check for lumps, swelling, or changes in the testicles. Early detection improves treatment outcomes and reduces the risk of long-term fertility issues.
Routine Medical Check-Ups
Regular check-ups with a healthcare provider can also aid in early detection. Men should discuss any changes or symptoms with their doctor promptly. Routine screenings and discussions about fertility preservation options should be part of the care plan for those diagnosed with testicular cancer.
Coping with Infertility
Emotional Support
Coping with potential infertility can be challenging. Emotional support from family, friends, and healthcare professionals is crucial. Counseling and support groups can provide a space for men to discuss their concerns and experiences.
Exploring Alternatives
For those who face infertility after treatment, exploring alternatives such as adoption or sperm donation can be considered. These options provide pathways to parenthood and can be fulfilling alternatives to biological reproduction.
Conclusion
Testicular cancer can impact fertility, but it does not necessarily cause sterility. The extent of the impact depends on the type and stage of cancer, the treatments used, and individual factors. Many men retain their fertility or regain it after treatment. Advances in fertility preservation techniques, such as sperm banking and assisted reproductive technologies, provide hope and options for men diagnosed with testicular cancer. Early detection, proactive fertility preservation measures, and comprehensive care can significantly mitigate the impact on fertility, allowing many men to achieve their dreams of fatherhood.
Related Links: