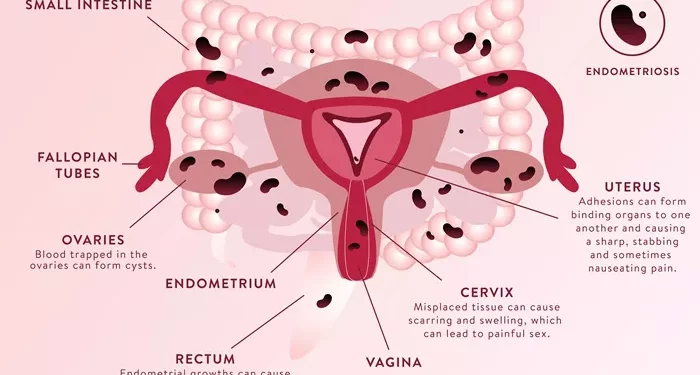
Endometriosis is a complex and often misunderstood condition that affects millions of women worldwide. It occurs when tissue similar to the lining of the uterus, called the endometrium, starts to grow outside the uterus. This aberrant tissue can be found on the ovaries, fallopian tubes, outer surface of the uterus, and other organs within the pelvis. The condition is often associated with chronic pelvic pain, heavy menstrual periods, and, significantly, impaired fertility.
Endometriosis is a leading cause of infertility in women. Studies suggest that 30% to 50% of women with endometriosis may experience difficulty getting pregnant. However, the relationship between endometriosis and infertility is multifaceted, involving a combination of anatomical, hormonal, and immunological factors. This article aims to provide a detailed understanding of how endometriosis affects fertility, the mechanisms involved, and the available treatment options.
The Prevalence of Endometriosis and Infertility
Endometriosis is a prevalent condition, affecting about 10% of women of reproductive age. Despite its commonality, the exact cause of endometriosis remains unknown. Some theories suggest that retrograde menstruation (when menstrual blood flows backward through the fallopian tubes into the pelvic cavity) may play a role, but this does not explain all cases.
Infertility is defined as the inability to conceive after one year of regular, unprotected intercourse. For women over 35, this timeframe is reduced to six months. Given that endometriosis is a leading cause of infertility, understanding its impact is crucial for both women seeking to conceive and healthcare providers managing their care.
How Endometriosis Affects Fertility
1. Anatomical Distortions
One of the most direct ways endometriosis affects fertility is through anatomical distortions of the reproductive organs. The abnormal growth of endometrial-like tissue can cause adhesions, scar tissue, and cysts, particularly on the ovaries and fallopian tubes.
Adhesions: Adhesions are bands of scar tissue that can cause organs to stick together. In the context of endometriosis, adhesions may form between the ovaries, fallopian tubes, and other pelvic organs. These adhesions can distort the normal anatomy, making it difficult for the egg to travel from the ovary through the fallopian tube and into the uterus for fertilization.
Ovarian Cysts: Also known as endometriomas or “chocolate cysts,” these are cysts that form when the endometrial tissue grows on the ovaries. These cysts are filled with old, dark blood and can cause significant damage to the ovarian tissue. This damage can reduce the ovarian reserve, which is the number of healthy eggs available for fertilization.
Fallopian Tube Damage: Endometriosis can also lead to the formation of scar tissue in or around the fallopian tubes. This damage can block the tubes, preventing the sperm from reaching the egg or the fertilized egg from reaching the uterus. Even if the tubes are not entirely blocked, any distortion can significantly reduce the chances of successful conception.
2. Ovulatory Dysfunction
Endometriosis can interfere with normal ovulation, making it more difficult for a woman to conceive. Ovulation is the process where a mature egg is released from the ovary and is available for fertilization. In women with endometriosis, this process can be disrupted in several ways:
Hormonal Imbalance: Endometriosis is associated with an imbalance in reproductive hormones, particularly estrogen and progesterone. This imbalance can affect the regularity and quality of ovulation. For instance, high levels of estrogen can lead to the formation of ovarian cysts and reduce the effectiveness of ovulation.
Inflammation: Chronic inflammation is a hallmark of endometriosis. The inflammatory environment in the pelvis can affect the ovaries, leading to the production of poor-quality eggs. Inflammation can also disrupt the function of the follicle-stimulating hormone (FSH), which is essential for egg maturation.
Reduced Ovarian Reserve: Women with endometriosis, particularly those with endometriomas, often have a reduced ovarian reserve. This means they have fewer eggs available for fertilization, which can significantly impact their fertility.
See also: Why Haven’t I Gotten Pregnant After Trying for 8 Months?
3. Impaired Egg Quality
Egg quality is a critical factor in fertility. Poor egg quality can lead to unsuccessful fertilization or failure of the embryo to implant in the uterus. Endometriosis is known to negatively affect egg quality through several mechanisms:
Oxidative Stress: The inflammatory environment created by endometriosis can lead to oxidative stress in the ovaries. Oxidative stress damages the DNA in the eggs, leading to poor egg quality and reducing the likelihood of successful conception.
Altered Follicular Environment: The follicles, which are the structures in the ovaries that contain the eggs, may be affected by endometriosis. The fluid within the follicles in women with endometriosis has been found to contain higher levels of inflammatory markers and other substances that can impair egg development and maturation.
Impact on Mitochondria: Mitochondria are the powerhouses of the cell and are crucial for the energy production needed for the egg’s development and maturation. Endometriosis-related inflammation and oxidative stress can damage the mitochondria within the eggs, further reducing egg quality.
4. Impaired Fertilization and Embryo Development
Even if ovulation occurs and the egg is released, endometriosis can still affect the fertilization process and subsequent embryo development. This can happen in several ways:
Sperm-Egg Interaction: The inflammatory environment in the pelvis can negatively affect sperm function. Sperm may struggle to reach the egg, or if they do, the inflammatory environment may reduce their ability to fertilize the egg successfully.
Embryo Quality: If fertilization occurs, the resulting embryo may be of poor quality due to the compromised egg and sperm quality. Poor-quality embryos are less likely to implant successfully in the uterus and are more likely to result in miscarriage.
Altered Uterine Environment: The presence of endometrial-like tissue outside the uterus can lead to an altered uterine environment. The inflammatory mediators produced by endometriosis can interfere with the process of implantation, making it difficult for the embryo to implant in the uterine lining.
5. Immunological Factors
Endometriosis is often associated with immune system dysregulation. The immune system plays a crucial role in reproduction, from sperm survival to embryo implantation. In women with endometriosis, several immunological factors can impair fertility:
Autoimmune Response: Some researchers believe that endometriosis may trigger an autoimmune response in the body. This response can lead to the production of antibodies that attack sperm, eggs, or embryos, making conception difficult or impossible.
Natural Killer Cells: Natural killer (NK) cells are a type of immune cell that plays a role in recognizing and destroying abnormal cells, including potential threats like infections. In women with endometriosis, NK cell activity may be altered, leading to an increased likelihood of embryo rejection during implantation.
Cytokines: Cytokines are signaling molecules that regulate immune responses. In women with endometriosis, the levels of certain cytokines may be elevated, creating an inflammatory environment that is hostile to sperm, eggs, and embryos.
6. Endometriosis Staging and Fertility Impact
Endometriosis is classified into four stages, depending on the extent and severity of the disease: minimal (stage I), mild (stage II), moderate (stage III), and severe (stage IV). These stages are based on factors such as the location, extent, depth, and size of the endometrial implants, as well as the presence of adhesions and endometriomas.
Stage I and II: In the early stages of endometriosis, the impact on fertility is usually less severe. However, even minimal or mild endometriosis can lead to subtle changes in the pelvic environment, which can impair fertility. Women with stage I or II endometriosis may still experience difficulty conceiving, but their chances of spontaneous pregnancy are generally better than those with more advanced stages.
Stage III and IV: In the more advanced stages of endometriosis, the anatomical distortions, adhesions, and ovarian damage are more pronounced. Women with stage III or IV endometriosis are more likely to experience infertility, and their chances of conceiving without medical intervention are significantly reduced. These women may require more aggressive fertility treatments, such as in vitro fertilization (IVF).
Diagnosing Endometriosis in Infertility
Diagnosing endometriosis can be challenging, especially in women who are asymptomatic or have minimal symptoms. However, for those experiencing infertility, a thorough evaluation is essential.
1. Medical History and Physical Examination
A detailed medical history and pelvic examination are the first steps in diagnosing endometriosis. The doctor will inquire about symptoms such as pelvic pain, painful periods, pain during intercourse, and infertility. During the pelvic examination, the doctor may feel for abnormalities such as cysts or tender areas, which could indicate the presence of endometriosis.
2. Imaging Studies
Imaging studies, such as ultrasound or magnetic resonance imaging (MRI), can help detect ovarian cysts (endometriomas) and other abnormalities associated with endometriosis. However, imaging alone cannot confirm the diagnosis of endometriosis, especially in cases where the disease is mild or there are no visible cysts.
3. Laparoscopy
Laparoscopy is the gold standard for diagnosing endometriosis. It is a minimally invasive surgical procedure in which a small camera (laparoscope) is inserted into the pelvic cavity through a small incision. This allows the doctor to directly visualize the endometrial implants and adhesions. During laparoscopy, the surgeon may also take tissue samples (biopsies) for further analysis and, in some cases, remove the endometrial lesions.
4. Fertility Testing
In addition to diagnosing endometriosis, women experiencing infertility may undergo other fertility tests. These can include hormone level testing, ovarian reserve assessment, and hysterosalpingography (an X-ray test that examines the inside of the uterus and fallopian tubes). These tests help determine the extent to which endometriosis is affecting fertility and guide treatment decisions.
Treatment Options for Endometriosis-Related Infertility
Treating endometriosis-related infertility requires a personalized approach, taking into account the severity of the disease, the woman’s age, overall health, and reproductive goals.
1. Medical Management
Hormonal Therapy: Hormonal treatments, such as birth control pills, gonadotropin-releasing hormone (GnRH) agonists, and progestins, can help reduce the symptoms of endometriosis by suppressing ovulation and menstruation. However, these treatments do not cure endometriosis and are not suitable for women actively trying to conceive, as they prevent pregnancy.
Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) and other pain-relieving medications can help manage the pain associated with endometriosis. While these treatments do not address infertility directly, they can improve the quality of life for women with endometriosis.
2. Surgical Treatment
Surgical intervention is often recommended for women with moderate to severe endometriosis, particularly when infertility is a concern. Surgery aims to remove as much endometrial tissue and adhesions as possible, restore normal pelvic anatomy, and improve the chances of conception.
Laparoscopic Surgery: Laparoscopic surgery is the preferred method for treating endometriosis. During the procedure, the surgeon removes or destroys endometrial implants, cysts, and adhesions. This can help restore normal anatomy and improve fertility. Studies have shown that surgical treatment of endometriosis can increase pregnancy rates, especially in women with stage I or II disease.
Ovarian Cystectomy: For women with endometriomas, surgical removal of the cysts (cystectomy) can improve fertility outcomes. However, it is essential to balance the removal of the cysts with the preservation of healthy ovarian tissue to maintain ovarian reserve.
3. Assisted Reproductive Technologies (ART)
For women with endometriosis who continue to struggle with infertility despite medical or surgical treatment, assisted reproductive technologies (ART) such as in vitro fertilization (IVF) may be recommended.
In Vitro Fertilization (IVF): IVF is the most effective ART for women with endometriosis-related infertility. The process involves stimulating the ovaries to produce multiple eggs, retrieving the eggs, fertilizing them with sperm in the laboratory, and transferring the resulting embryos into the uterus. IVF bypasses many of the barriers to conception associated with endometriosis, such as tubal damage and poor egg quality.
Intracytoplasmic Sperm Injection (ICSI): ICSI is a technique often used in conjunction with IVF, where a single sperm is injected directly into an egg to facilitate fertilization. ICSI can be particularly beneficial for couples where male infertility is also a factor.
Egg Donation: In cases where endometriosis has severely compromised ovarian reserve and egg quality, egg donation may be an option. This involves using eggs from a donor, which are fertilized with the partner’s sperm and transferred to the recipient’s uterus.
4. Fertility Preservation
For women diagnosed with endometriosis who are not yet ready to conceive, fertility preservation options such as egg or embryo freezing (cryopreservation) can be considered. This is particularly important for women with a significant risk of reduced ovarian reserve due to endometriosis or planned surgical intervention.
Prognosis and Future Outlook
The prognosis for fertility in women with endometriosis varies widely depending on the severity of the disease, age, and overall reproductive health. While endometriosis can significantly impact fertility, many women with the condition can still conceive and have successful pregnancies, either naturally or with medical assistance.
1. Spontaneous Pregnancy Rates
Spontaneous pregnancy rates in women with endometriosis vary. Women with minimal or mild endometriosis have a better chance of conceiving naturally, while those with more severe disease often require medical or surgical intervention. Studies suggest that the removal of endometriosis lesions can improve spontaneous pregnancy rates, especially in women with mild to moderate disease.
2. Success Rates with Assisted Reproductive Technologies
The success rates of ART, particularly IVF, in women with endometriosis are generally lower than in women without the condition. However, advancements in reproductive medicine, such as improved ovarian stimulation protocols and the use of preimplantation genetic testing, have helped improve outcomes for women with endometriosis.
3. Recurrence and Long-Term Management
Endometriosis is a chronic condition, and recurrence is common, even after surgical treatment. Long-term management of endometriosis may involve a combination of medical treatment, lifestyle modifications, and, when appropriate, fertility preservation strategies. Women with endometriosis should work closely with their healthcare providers to develop an individualized plan that addresses both symptom management and fertility preservation.
Conclusion
Endometriosis is a significant and complex cause of infertility, affecting multiple aspects of the reproductive system. While the condition presents many challenges, a range of medical, surgical, and assisted reproductive options are available to help women with endometriosis achieve their fertility goals. Early diagnosis and a tailored treatment approach are key to improving fertility outcomes and enhancing the quality of life for women with this condition. Women with endometriosis who are trying to conceive should seek guidance from a reproductive specialist to explore the best options for their individual circumstances.
Related topics: